How does the eye tissue donation process work?

The Donor Registry
The Colorado and Wyoming donor registries are confidential databases of the people in those states who signed up to be eye, organ, and tissue donors. In Colorado, about 67% of the adult population that has a driver's license or ID is registered to be a donor. In Wyoming, about 61% are registered. These are some of the highest registry rates in the nation.
The Uniform Anatomical Gift Act (UAGA), which established the registry and guides the donation process, was passed by the Colorado legislature in 1998. The UAGA in Colorado has been updated many times, with the last revision in 2017. Wyoming adopted the UAGA several years after Colorado. Registering on the donor registry is legal consent under the law, and if the donor did not remove their registration prior to death, the law bars anyone from reversing the donor's decision to donate after death. When a potential donor is not registered, his or her legal next-of-kin makes the decision on their behalf. Note the UAGA specifies a list of who is the next-of-kin that may give authorization.
Anyone can sign up to be a donor in their state's donor registry regardless of age, health, or lifestyle. Even people with chronic medical conditions and infectious diseases may be able to donate.
Screening and Evaluation of Cornea Donors
Donors are initially screened during the referral call. Hospitals have a federal mandate to report all deaths for donation eligibility determination. The eye bank will also look at the patient's medical records for anything that might rule out the donor. Once eligibility is determined, registry verified or authorization for donation is obtained, our staff will coordinate with other recovery agencies and, if necessary, the coroner prior to recovery.
The recovery procedure is performed by a single recovery technician, who will conduct a thorough, gross penlight exam of the eyes, looking for any conditions that might be of concern. The technician will also perform a body exam prior to recovery. The recovery procedure is done aseptically using a sterile field and is very much like surgery. In fact, we use some of the same kinds of surgical instruments the transplanting surgeon will use.
 Once the recovered eye tissue is at the eye bank, we look at it under a slit-lamp microscope to evaluate its condition. This is the same instrument your ophthalmologist uses to examine your cornea during an eye exam. This microscope allows us to look at the various layers of the cornea for any abnormalities. Because the cornea is transparent, most abnormalities cannot be seen with the naked eye.
Once the recovered eye tissue is at the eye bank, we look at it under a slit-lamp microscope to evaluate its condition. This is the same instrument your ophthalmologist uses to examine your cornea during an eye exam. This microscope allows us to look at the various layers of the cornea for any abnormalities. Because the cornea is transparent, most abnormalities cannot be seen with the naked eye.
The next step uses another specialized microscope: a specular microscope. This analysis looks more closely at the endothelial cells on the back of the cornea. It allows us to count the cells and to assess the general health of the endothelial layer.
Finally, several tests will be performed on the donor's blood to ensure the absence of a variety of transmissible diseases. These tests are mandated by the Food and Drug Administration (FDA). Sometimes, coroners will be asked to share blood samples with the eye bank so this critical step can be completed.
Corneal Transplantation
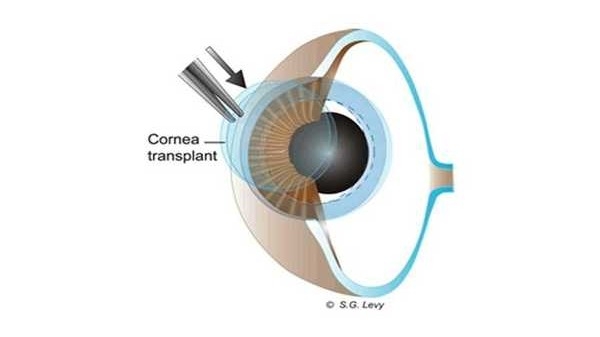
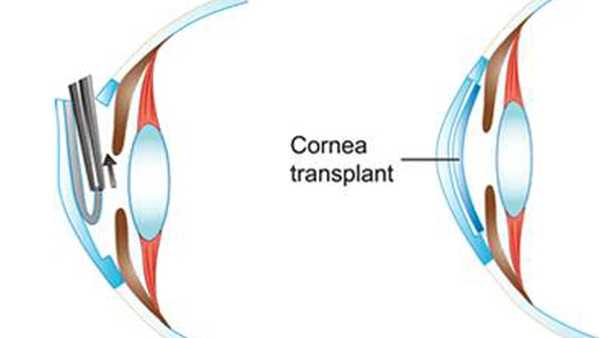
A diseased or damaged cornea is removed from the recipient using a trephine, a circular cutting instrument.
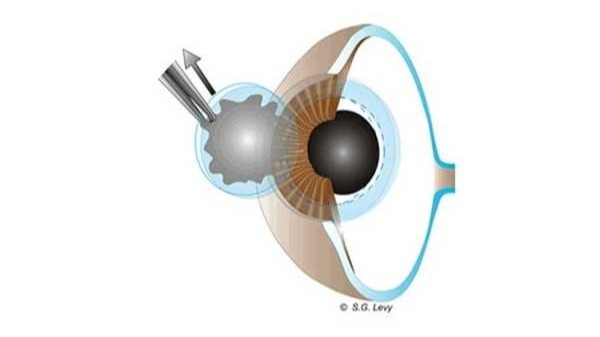
A similarly sized graft from the donor cornea is made in the same manner and then placed into the recipient's eye. The diameter of the graft is determined by the eye bank during the microscopic examination of the donor's cornea. The graft is put into place by hand using microfilament sutures.
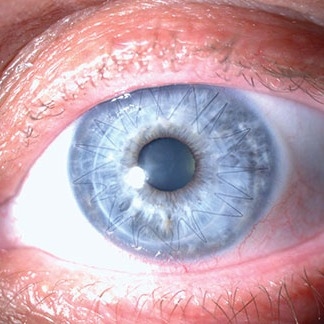
Here is the result:
Another, newer procedure, Descemet Membrane Endothelial Keratoplasty (DMEK), transplants just the endothelial layer of the cornea. This allows the eye bank to transplant corneas that otherwise couldn't be used. For example, if the cornea is scratched heavily because of trauma in a car accident, the eye bank can split the cornea lengthwise and transplant just the back half for certain recipients who have diseases of the endothelium. The highly technical procedure is done at the eye bank in special procedure rooms that meet strict international standards.
After the eye bank removes the outer portion of the donor cornea in the lab, the resulting endothelial graft is extremely thin. The photo below on the right is taken by an optical coherence tomography of the split graft of the donor cornea. It is only 65 microns thick, but these grafts can be as thin as 10-15 microns. By comparison, a human hair averages 180 microns in diameter.

In surgery, the recipient's endothelium is removed through a small incision in the periphery of their cornea and the new, very thin endothelial graft is placed inside. There are no stitches, and many patients see 20/20 within a few days.
.
This video shows an ultra-thin DMEK graft being prepared at the Rocky Mountain Lions Eye Bank for a surgeon to use in a procedure: